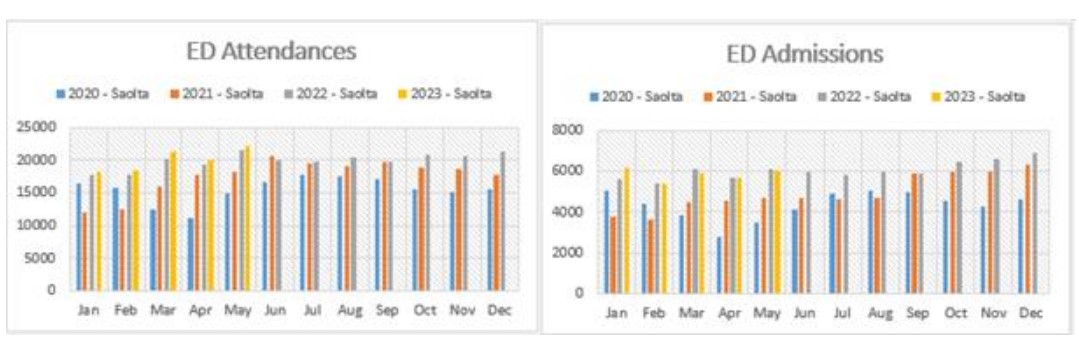
The Deputy Chairperson of the Regional Health Forum West says Saolta and the HSE’s efforts to improve patient flow at Letterkenny University Hospital must be acknowledged, but is stressing it is very much a work in progress.
Officials told Cllr Ciaran Brogan in reply to questions that a Local Injury Unit is operational in the Emergency Department, and it’s hoped that can be enhanced as part of the Winter Plan.
Liaison officers are being appointed, measures are being introduced to help people and the Pathfinder initiative is helping keep people out of hospital by treating them in their own homes.
Cllr Brogan says the more people that can be kept out of hospital, the better……….
Reply in full –
The Emergency Department has developed a number of Pathways aimed at reducing the patient’s time spent in the
Emergency Department.
Local Injury Unit – operational since 9th May 2022. A “Purple Pathway” has been established within existing resources, this is
an ambulatory stream created in ED which provides a protected space where Advanced Nurse Practitioners and an Emergency
Doctor Registrar review patients with minor injury assessment and provide treatment.
This has been working well with direct streaming from triage. LUH in conjunction with CHO1 has made a submission for further
funding to extend the opening hours of this local injury unit as part of the Winter Plan.
Portering – An additional porter has been rostered to the Emergency Department to assist with admission and timely
movements for diagnostics.
PALS –Patient Advice & Liaison Service – Two posts have been recruited. One PALS officer has commenced in LUH with the
second currently awaiting clearance.
Frailty at the Front Door service is also in place in the Emergency Department. This teams assess patients over the age of 75
years with the aim to identify patients in need of frailty support or/and further assessment. It carries out a comprehensive
assessment on older people reviewing alternative pathways to avoid admission or to allow early discharge.
The Emergency Department has also developed a number of Admission Avoidance Pathways including a Stable Chest Pain
Pathway and a Stable Upper GI Bleed Pathway.
Chest Pain Pathway- operational since 25th April 2022. The Cardiac Investigation Department have ringfenced 2 slots for
Exercise Stress Tests per day. This streamlines the pathway for patients presenting at ED with chest pains and has resulted
in a reduction of admissions.
Stable Upper GI Bleed- operational since 20th May 2022. Patients are triaged as per the Glasgow-Blatchford Score, which
stratifies upper GI bleeding patients who are ‘low-risk’ and candidates for outpatient management.
The Pathfinder Service was also introduced recently. This service assesses lower acuity ambulance calls in the Community and
arranges/recommends alternative health care whenever appropriate. The new service aims to safely keep vulnerable older
people who have phoned 999/112, in their own home rather than transporting them to the ED for assessment. A specific
team of staff are employed to deliver this service including Advanced Paramedics (AP), Occupational Therapists (OT) and
Physiotherapists (PT); will include a Rapid Response Vehicle (RRV) and an Electronic Patient Care Record (EPCR).
LUH is working closely with both Community Healthcare Organisation, (Cavan, Donegal, Leitrim, Monaghan, Sligo) and NAS to
ensure all available care options are utilised and patients are directed to and provided with the proper care pathway. There is also significant work taking place to progress discharges and treat patients in the community. This work includes liaising
with Community-Based Health Care Professionals about Delayed Transfers of Care from Letterkenny University Hospital,
development of a future OPATs service and the Community Intervention Team Referrals.
This conjoined working is well established and has led to a wide range of care options which are further outlined below.
Donegal Primary Care interface working with Letterkenny University Hospital (LUH) to improve patient flow.
Community Diagnostics
Some 4,900 X-rays have been carried out at the five newly-refurbished community X-ray facilities to date this year.
Plain film X-rays are being completed for repeat outpatient appointments to support care closer to the person’s home.
Unscheduled Care meetings are attended by senior staff from Primary Care, including the Head of Service CHO1,
Donegal General Manager, Director of Public Health Nursing and members of the Community Intervention Team (CIT),
Integrated Care Programme for Older Persons (ICPOP) and Chronic Disease Management (CDM) team to review the
flow of unscheduled care in LUH.
Palliative Care In-reach and Outpatients
Consultants from Donegal Hospice carry out daily rounds in LUH and additional outpatients clinics are held with the
LUH Oncology team.
Integrated Discharge Planning Rounds: Primary Care staff, ICPOP, CIT and PHN services are represented in the weekly
integrated discharge planning rounds. The Donegal Primary Care General Manager’s office also reviews the daily lists
of the Delayed Transfers of care.
Community Intervention Teams (CITs)
The CITs facilitate acute, short-term nursing interventions, including wound management, oncology care, medication
administration and management, patient education and support, to promote self-management of catheters and
stoma care.
CIT staff attend a weekly Integrated Discharge Round (IDR) in LUH to identify patients who are suitable for early
discharge and who meet the criteria for CIT care. The IDR also promotes early discharge planning for complex patients
and creates a clear plan of care for the PC teams involved in the patient’s discharge.
Chronic Disease Management Donegal
Cardiology – Heart Failure – Primary Care nursing staff, i.e. Advanced Nurse Practitioner (ANP), Clinical Nurse
Specialist (CNS); Diagnostic ECHO service – direct referral from GPs
Cardiac Rehab Coordinator supported by Primary Care physiotherapists
Supporting LUH cardiac rehab service as there is no clinical governance to commence community service at present.
Diabetes
Dietetics – supported by Primary Care ANP and CNS; Podiatry service, Dietetic service; Type 2 Diabetes Digital Media
1:1 consultations operational; DESMOND education, Diabetes Prevention Programme and Best Health weight
management programmes.
Integrated Endocrinology Consultants in post
Respiratory
Assessment clinics – inhaler review, airways clearance
Pulmonary Rehabilitation
O2 clinics
Non-acute respiratory symptoms management clinic
Pulmonary Rehabilitation education
Community Diagnostic Heart Failure services
Reduction in LUH Cardiac out-patient wait list of 114 people as a result of ongoing review of LUH OPD Cardiology list
by the Cardiac Physiologist with notifications to the Cardiac Investigations Department, LUH to advise of those
patients who have had an ECHO completed.
NowDOC
In times of a surge additional GP’s & Nursing staff are put in place.
Additional GP’s & Nursing staff are also put in place for Bank Holidays and large scale events.
Dermot Monaghan, Chief Officer, Community Healthcare Organisation, (Cavan, Donegal, Leitrim, Monaghan, Sligo)
Continuous extensive engagement continues on a daily basis between the National Ambulance Service (NAS) and Hospitals in
relation to ambulance to hospital (A2H) delays. In addition various steps have been introduced to alleviate the issue. The steps
include:
Hospital Ambulance Liaison Person (HALP) – The aim of this role is to work between the hospital and the ambulance
service in order to have ambulance turned around in a more efficient manner. To date we have seen a positive impact
for this role and will continue to monitor its progress over the coming period as per question W106Q3743 this role
has been extended for the remainder of 2023 and we are seeking permanent funding for same.
Fit2Sit – where patients are capable of sitting, then crews will focus on finding a safe place for the patient and effecting
a clinical handover as quickly as possible
Rapid Handover Protocol – the current arrangements are not effective and in this regard, crews will be provided with
revised protocols on how to be more proactive in effecting patient disposition at the Emergency Department in a
timely manner. The Rapid Handover Protocol will provide for red flagging of sites where A2H delays present a real risk
of harm to patients awaiting a 999 response in the community.
NAS Cohorting – where necessary and in the absence of clear clinical governance of patients awaiting clinical
handover in the Emergency Department, NAS will request staff to engage in cohorting of patients at Emergency
Departments to facilitate release of an emergency ambulance to respond to an awaiting 999 call. Crews will be
provided with guidelines on how to do this safely.